With the inGAGE™ HRA workflow automation, you will:
Improvement in HRA completion rate YoY
Increase in case management engagement for members who completed the HRA
Net cost avoidance in the first year
Cost savings YoY

Learn how a regional Blues plan serving Medicaid and dually-eligible members used inGAGE™ to address low HRA completions and drive Next Best Actions.
Let’s TalkWith inGAGE™ you will understand where you are with your HRA completions at all times. This real-time insight allows you to:
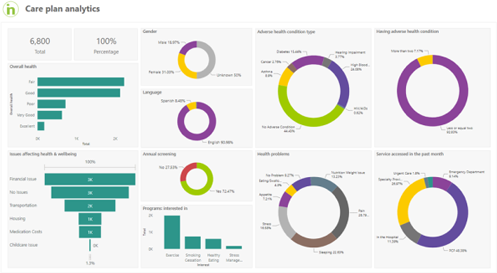
This level of reporting gives you the information you need to reach your compliance goals and impact Stars measures.
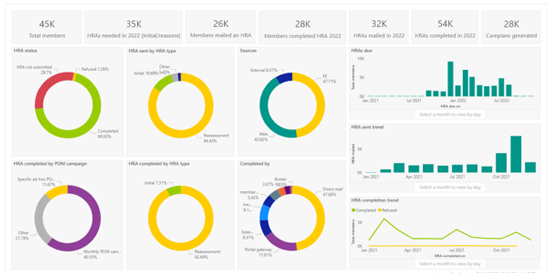

The inGAGE™ artificial intelligence and machine learning determines the influencing factors that impact HRA completions. Knowing this, you can:
By understanding the influencing factors, you can also take effective actions to get HRA completions earlier in the year – which provides opportunities to address access to care barriers and member engagement sooner than later.
With insight into how members are responding to the HRA, inGAGE™ can trigger automated Next Best Actions to promptly address member needs. For example:
Additionally, member HRAs and care plans are always accessible via inGAGE™ and can be seamlessly transferred to care management systems, member portals and provider portals – you name it – enabling a total member experience.