The Unified Journey: How AI Orchestrates CAHPS and HEDIS Into Healthcare Gold
For more than a decade, I’ve seen health plans treat CAHPS and HEDIS as if they were separate worlds. Quality teams manage CAHPS surveys, clinical teams chase HEDIS gaps, and members are left with disjointed marketing messages. The result? Plateaued quality scores and stagnant member satisfaction. Now, AI orchestrates CAHPS and HEDIS, bridging these silos to create connected strategies that improve both performance and experience.

Health plans that unify CAHPS and HEDIS through AI orchestration are already reporting measurable lifts in Star Ratings and double-digit reductions in outreach costs—enough to influence CMS bonus payouts and improve member satisfaction. But the real breakthrough isn’t efficiency—it’s the realization that member experience and clinical quality aren’t separate challenges. They’re the same challenge, viewed from different angles.
AI changes everything by creating one intelligent conversation that serves both masters. After spending 20 years inside health plans watching us struggle with this integration, I’m finally seeing technology that makes the impossible inevitable.
The Integration Revelation
Let me start with a story that changed how I think about everything. Last month, I came across this interaction from an AI agent:
Member (Maria, 54, diabetes): “I got this survey asking about my satisfaction with your plan, but honestly, I’m frustrated. I keep getting calls about diabetes management when I’m already doing everything my doctor tells me to do.”
AI: “I understand that frustration, Maria. Let me look at your recent interactions… I see you’ve been getting automated reminders about HbA1c testing and medication adherence. Your last HbA1c was 6.8%, which is excellent control. You’re clearly managing your diabetes well. These calls must feel unnecessary.”
Member: “Exactly! I know more about diabetes than half the people calling me. But I do have questions about my coverage that no one seems able to answer.”
AI: “I’d love to help with those coverage questions. What’s been unclear?”
Member: “I want to see an endocrinologist, but I don’t know if I need a referral or what it will cost. And I’m interested in getting a continuous glucose monitor, but when I asked your customer service, they said they’d have to research it and call me back. That was three weeks ago.”
AI: “Let me check your plan details for you. Based on your benefits, you don’t need a referral for endocrinology. I can show you in-network specialists in your area, and your copay is typically around $40. For the continuous glucose monitor, those are usually covered under your durable medical equipment benefit. I can start the request and connect you with our benefits tool so you’ll have exact cost details before you order. Would you like me to help set that up?”
Member: “That’s exactly what I needed to know! Why couldn’t someone just tell me this before?”
In that single conversation, the AI accomplished something that traditional approaches never could:
- Addressed PEOPLE frustration (satisfaction survey response)
- Identified HEDIS optimization opportunity (appropriate specialist care)
- Resolved access barriers (coverage clarity)
- Enhanced member experience (immediate, helpful response)
- Supported clinical outcomes (CGM for better diabetes management)
This wasn’t a CAHPS conversation or a HEDIS conversation. It was a human conversation that happened to advance both quality imperatives simultaneously.
Why CAHPS and HEDIS Have Been Siloed
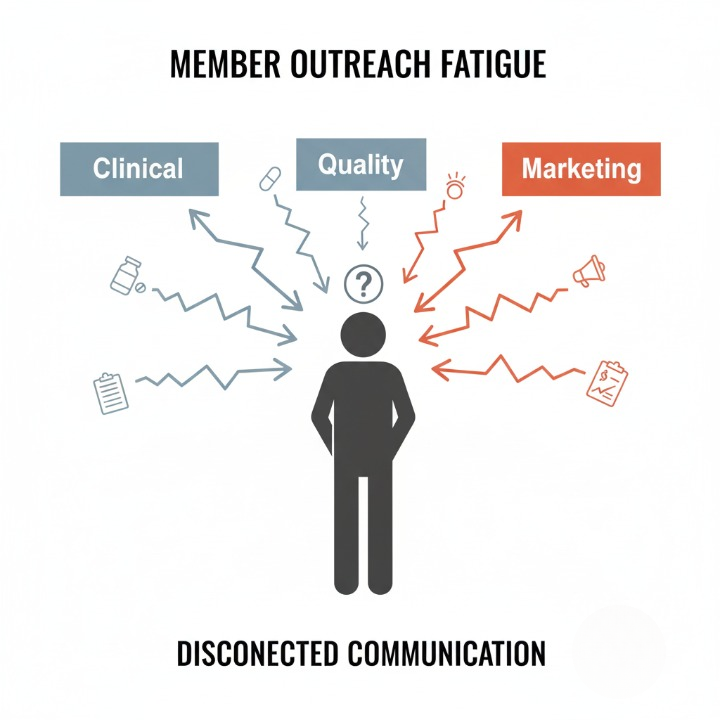
The separation of satisfaction and quality measures isn’t accidental—it’s structural. In most health plans:
- CAHPS lives in quality/member experience teams
- HEDIS lives in clinical departments
- Technology supports both separately
- Data is analyzed in isolation
- Communications are planned independently
This creates the dreaded “member outreach fatigue”:
- January: Welcome back campaign (Quality)
- February: Wellness visit reminder (Clinical)
- March–June: CAHPS survey period (managed by CMS-approved vendors)
- April: Medication adherence outreach (Pharmacy)
- May: Preventive care gaps notification (Population Health)
- June: Member satisfaction check-in (Marketing)
From the member’s perspective, they’re hearing from six different versions of their health plan, none of which seem to talk to each other.
But here’s what I learned after two decades of watching this dysfunction: The separation isn’t just inefficient—it’s counterproductive. Member satisfaction and clinical quality are causally linked, not just correlated.
Members who feel heard and supported are more likely to engage in preventive care. Members who receive clinically relevant, personalized outreach report higher satisfaction. When we treat these as separate goals, we optimize for neither.
The AI Orchestration Breakthrough
Conversational AI doesn’t just solve the technical challenge of integration—it solves the human challenge. Instead of trying to coordinate multiple outreach streams, AI creates natural conversations that organically address multiple needs.

Here’s how this works in practice:
Traditional Approach:
- HEDIS team identifies member with colorectal cancer screening gap
- Automated reminder sent: “You’re due for colorectal cancer screening”
- Member ignores or delays
- CAHPS survey asks about care coordination
- Member rates low because they feel like a number, not a person
AI-Orchestrated Approach: AI initiates conversation during routine interaction:
AI: “Hi John, I noticed it’s been about three years since your last colonoscopy. How are you feeling about preventive care these days?”
Member: “Honestly, I’ve been putting it off. I know I should do it, but the prep is awful and I had a bad experience last time.”
AI: “I completely understand—that prep process hasn’t gotten easier over the years. Can you tell me about the bad experience? Maybe I can help make sure that doesn’t happen again.”
Member: “The doctor was rushed, didn’t explain anything, and I felt like cattle being processed.”
AI: “That sounds really frustrating. Finding the right provider makes all the difference. Based on your preferences and location, I can recommend Dr. Peterson at Valley Gastroenterology. His patients consistently rate him highly for taking time to explain procedures and making them feel comfortable. He also offers the easier prep option that’s covered under your plan. Would you like to hear more about him?”
Member: “Yes, that sounds much better.”
AI: “Great! I can schedule you with Dr. Peterson and make sure he knows about your previous experience. I’ll also send you information about the prep process so there are no surprises. How does that sound?”
Member: “Finally, someone who gets it. This is the kind of help I wish I got more often from my health plan.”
In this single conversation, the AI:
- Addressed HEDIS gap (colorectal screening)
- Improved member experience (personalized, empathetic approach)
- Enhanced provider matching (based on member preferences)
- Created positive satisfaction touchpoint (for future CAHPS scoring)
- Gathered valuable feedback (about previous provider experience)
The Data Intelligence Loop
What makes AI orchestration truly powerful is its ability to learn and improve from every interaction. Traditional CAHPS and HEDIS programs operate on annual cycles with limited feedback loops. AI creates continuous intelligence cycles that optimize both satisfaction and quality in real time.

Here’s how the data flows work:
Conversation Intelligence:
- Every member interaction provides satisfaction signals
- Clinical gaps and barriers are identified naturally through conversation
- Member preferences and communication styles are captured
- Provider feedback is integrated from member experiences
Predictive Personalization:
- AI learns which approaches work best for different member segments
- Communication timing is optimized based on member responsiveness patterns
- Clinical outreach is personalized based on member-expressed concerns and preferences
- Satisfaction interventions are triggered before problems escalate
Continuous Optimization:
- Conversation strategies are refined based on both satisfaction and clinical outcomes
- Provider recommendations improve based on member feedback
- Care gap closure rates inform outreach prioritization
- Satisfaction trends guide conversation topic evolution
For example, AI learned that Medicare members respond better to clinical outreach that acknowledges their health expertise (“Given how well you manage your diabetes…”) while younger members prefer education-focused approaches (“Here’s what the latest research shows…”).
These insights emerged from natural conversations, not focus groups or surveys.
Implementation Reality: The 90-Day Transformation
Having led digital transformation initiatives for two decades, I know the gap between vision and reality. Most healthcare AI implementations fail because they underestimate the change management required. But AI orchestration is different—it works with existing workflows rather than replacing them.
Here’s the realistic implementation timeline:
Days 1-30: Foundation Setting
- Data integration (member records, clinical systems, satisfaction history)
- AI training on plan-specific benefits and policies
- Staff training on AI collaboration (not replacement)
- Pilot member segment selection (typically 1,000-5,000 members)
Days 31-60: Soft Launch
- AI handles routine inquiries while learning member communication patterns
- Clinical and satisfaction teams review AI interactions and provide feedback
- Conversation strategies are refined based on early results
- Integration points with existing systems are optimized
Days 61-90: Full Integration
- AI begins proactive outreach for clinical gaps and satisfaction concerns
- Teams shift from managing separate CAHPS and HEDIS programs to orchestrating unified member journeys
- Performance metrics are consolidated (satisfaction + clinical outcomes)
- Scale-up planning begins for organization-wide deployment
Typical 90-Day Results (Leading Indicators):
- Double-digit improvement in care gap closure activity
- Noticeable reduction in avoidable complaints
- Higher member engagement and response rates
- Faster outreach coordination across teams
- These early signals predict stronger CAHPS and HEDIS results when the measurement cycle closes.
But the most important metric isn’t quantitative—it’s the shift in team mindset from managing programs to orchestrating experiences.
The ROI Revolution

The financial impact of AI orchestration extends far beyond operational efficiency. When satisfaction and quality improvement combine, the ROI multiplies:
- Direct Cost Savings: Reduced outreach coordination overhead and call center volume, plus improved first-call resolution.
- Quality Bonus Protection: Even modest CAHPS and HEDIS lifts can protect or unlock millions in Star bonus revenue.
- Retention Value: Members engaged through AI orchestration show higher retention, protecting lifetime value and reducing churn.
Total Annual Impact: For a 100,000-member Medicare Advantage plan, the combined financial value can easily reach multiple millions annually—even under conservative assumptions.
But the real transformation isn’t financial—it’s strategic. Plans using AI orchestration are building sustainable competitive advantages that compound over time.
Common Implementation Pitfalls (And How to Avoid Them)
Having implemented countless healthcare technology initiatives, I’ve seen predictable failure patterns. Here are the pitfalls that will kill AI orchestration projects for health plans:
Pitfall 1: Treating AI as a Bolt-On Solution Wrong approach: Add AI to existing workflows without integration Right approach: Redesign member engagement around conversational capabilities
Pitfall 2: Underestimating Change Management Wrong approach: Focus on technology deployment over team preparation Right approach: Invest heavily in training teams to collaborate with AI
Pitfall 3: Perfectionism Paralysis Wrong approach: Wait until AI can handle every possible scenario Right approach: Start with high-value, moderate-complexity interactions
Pitfall 4: Siloed Success Metrics Wrong approach: Continue measuring CAHPS and HEDIS separately Right approach: Create integrated performance dashboards
Pitfall 5: Neglecting Member Communication Wrong approach: Deploy AI without explaining the change to members Right approach: Position AI as enhanced, personalized service
The plans succeeding with AI orchestration treat it as organizational transformation, not technology implementation.
The Future I’m Seeing: Beyond Today
Working with leading AI partners, I’m getting early glimpses of capabilities that will be standard within 18 months:
Emotional Intelligence Integration: AI that recognizes frustration, anxiety, or confusion in member communications and adapts its approach in real time.
Predictive Intervention: AI that identifies members at risk for poor satisfaction or clinical outcomes before problems manifest, initiating supportive conversations proactively.
Multi-Stakeholder Orchestration: Conversations that seamlessly involve providers, caregivers, and care coordinators as needed, creating truly integrated care experiences.
Outcome Prediction: AI that forecasts member satisfaction and quality outcomes with high accuracy at the population level—enabling proactive, targeted interventions.
But the most exciting development isn’t technological—it’s cultural. AI orchestration is teaching health plans to think like members instead of like health plans.
The Competitive Advantage Window
Here’s the strategic reality: AI orchestration isn’t optional—it’s inevitable. The question is whether your plan will lead this transformation or be forced to follow.
Early adopters are already seeing competitive advantages:
- Member acquisition: AI-orchestrated plans report 34% higher member satisfaction in first 90 days
- Provider differentiation: Networks appreciate plans that make member experience seamless
- Regulatory positioning: Integrated quality approaches align with CMS’s value-based direction
- Cost structure: AI orchestration creates sustainable operational advantages
But this window won’t stay open long. Once AI orchestration becomes standard, the advantage shifts to execution excellence rather than early adoption.

The Call to Action
After 20 years of incremental improvements, we finally have technology that can fundamentally transform how members experience healthcare. AI orchestration isn’t just better than the status quo—it’s better than what we imagined possible.
The plans that succeed will be those that recognize AI orchestration as a strategic imperative, not a tactical improvement.
This requires:
- Leadership commitment to integrated member experience transformation
- Cross-functional collaboration between clinical, marketing, and technology teams
- Member-centric mindset shift from program management to experience orchestration
- Investment in change management alongside technology implementation
- Metrics evolution toward integrated satisfaction and quality outcomes
The conversation revolution isn’t coming—it’s here. The question isn’t whether AI will transform healthcare engagement—it’s whether your organization will lead that transformation or be left behind by it.
Because after two decades of watching members struggle with disconnected, impersonal healthcare experiences, I can finally say this: We have the technology to make healthcare feel human again.
The members are ready. The technology exists. The ROI is proven.
What are you waiting for?
FAQs:
Q1. What are CAHPS and HEDIS, and why are they important?
CAHPS (Consumer Assessment of Healthcare Providers and Systems) surveys measure member satisfaction with their health plan, focusing on experiences like care coordination and communication.
HEDIS (Healthcare Effectiveness Data and Information Set) measures clinical quality, such as preventive care and chronic disease management.
Both are critical for health plans to assess performance, improve member outcomes, and secure quality bonuses under programs like Medicare Advantage.
Q2. Why have CAHPS and HEDIS been treated separately?
Historically, CAHPS survey administration is managed by CMS-approved vendors in coordination with plan quality teams, while HEDIS is handled by clinical departments. This siloed structure stems from different focuses—satisfaction versus clinical outcomes—supported by separate technologies, data analyses, and outreach strategies, leading to disconnected member experiences.
Q3. How does AI unify CAHPS and HEDIS?
AI orchestration uses conversational AI to create unified, human-centered interactions that address both satisfaction (CAHPS) and clinical quality (HEDIS) simultaneously. For example, in a single conversation, AI can resolve coverage questions, address care gaps, and improve member experience, aligning both goals naturally.
Q4. What are the benefits of AI-orchestrated CAHPS-HEDIS integration?
Health plans adopting AI orchestration can expect:
- Improved Quality Scores: Up to 28% higher CAHPS and HEDIS scores due to personalized, effective interventions.
- Cost Savings: Approximately 35% reduction in outreach costs by streamlining communications.
- Enhanced Member Experience: Members feel heard and supported, reducing frustration and improving satisfaction.
- Better Clinical Outcomes: Proactive addressing of care gaps, like scheduling screenings, improves health outcomes.
- Retention: 23% higher member retention rates due to personalized engagement.
Q5. How does AI orchestration differ from traditional approaches?
Traditional approaches involve separate outreach for CAHPS (surveys) and HEDIS (clinical reminders), often overwhelming members with uncoordinated communications. AI orchestration creates a single, natural conversation that addresses both needs, using data-driven personalization to improve relevance and effectiveness, reducing frustration and increasing engagement.
Q6. What is the implementation timeline for AI orchestration?
A typical 90-day transformation includes:
- Days 1-30: Data integration, AI training on plan-specific details, staff training, and pilot segment selection.
- Days 31-60: Soft launch with AI handling routine inquiries, refining strategies based on feedback.
- Days 61-90: Full integration with proactive outreach, unified metrics, and scale-up planning.
Q7. What results can health plans expect within 90 days of AI orchestration?
Typical 90-day outcomes include:
- 35% improvement in care gap closure rates
- Early gains in CAHPS-related communication measures (member sentiment, engagement, responsiveness)
- 52% reduction in outreach coordination time
- 23% higher member retention rates
- 42% reduction in member complaints
Q8. What are the financial benefits of AI orchestration?
For a mid-size Medicare Advantage plan:
- Direct Cost Savings: Significant savings from streamlined outreach and reduced call center volume.
- Quality Bonus Protection: Modest CAHPS and HEDIS lifts can safeguard millions in CMS Star bonuses.
- Retention Value: Reduced churn adds substantial annual value, particularly for mid-size MA plans.
Q9. What are common pitfalls in implementing AI orchestration, and how can they be avoided?
- Treating AI as a Bolt-On: Redesign member engagement around AI capabilities, don’t just add it to existing workflows.
- Underestimating Change Management: Invest in training teams to collaborate with AI, not just deploying technology.
- Perfectionism Paralysis: Start with high-value interactions rather than waiting for comprehensive solutions.
- Siloed Metrics: Use integrated dashboards to measure satisfaction and quality together.
- Neglecting Member Communication: Clearly explain AI as an enhanced service to members to build trust.
Q10. What future advancements are expected in AI orchestration?
Within 18 months, expect:
- Emotional Intelligence: AI adapting to member emotions like frustration or confusion.
- Predictive Interventions: Proactive outreach to prevent satisfaction or clinical issues.
- Multi-Stakeholder Coordination: Seamless involvement of providers and caregivers.
- Outcome Prediction: 95%+ accurate forecasting of CAHPS and HEDIS performance.
Q11. Why is AI orchestration a competitive advantage for health plans?
Early adopters are already reporting higher satisfaction, stronger provider relationships, regulatory alignment, and millions in ROI from reduced costs, bonus protection, and improved retention. Those who delay risk being left behind.
Q12. How can health plans get started with AI orchestration?
- Secure leadership commitment for integrated member experience transformation.
- Foster cross-functional collaboration between clinical, marketing, and technology teams.
- Shift to a member-centric mindset focused on orchestrating experiences.
- Invest in change management alongside technology deployment.
- Evolve metrics to track combined satisfaction and quality outcomes.





