The Death of Menu-Driven Healthcare: Why 20 Years of ‘Click Here’ Isn’t Working
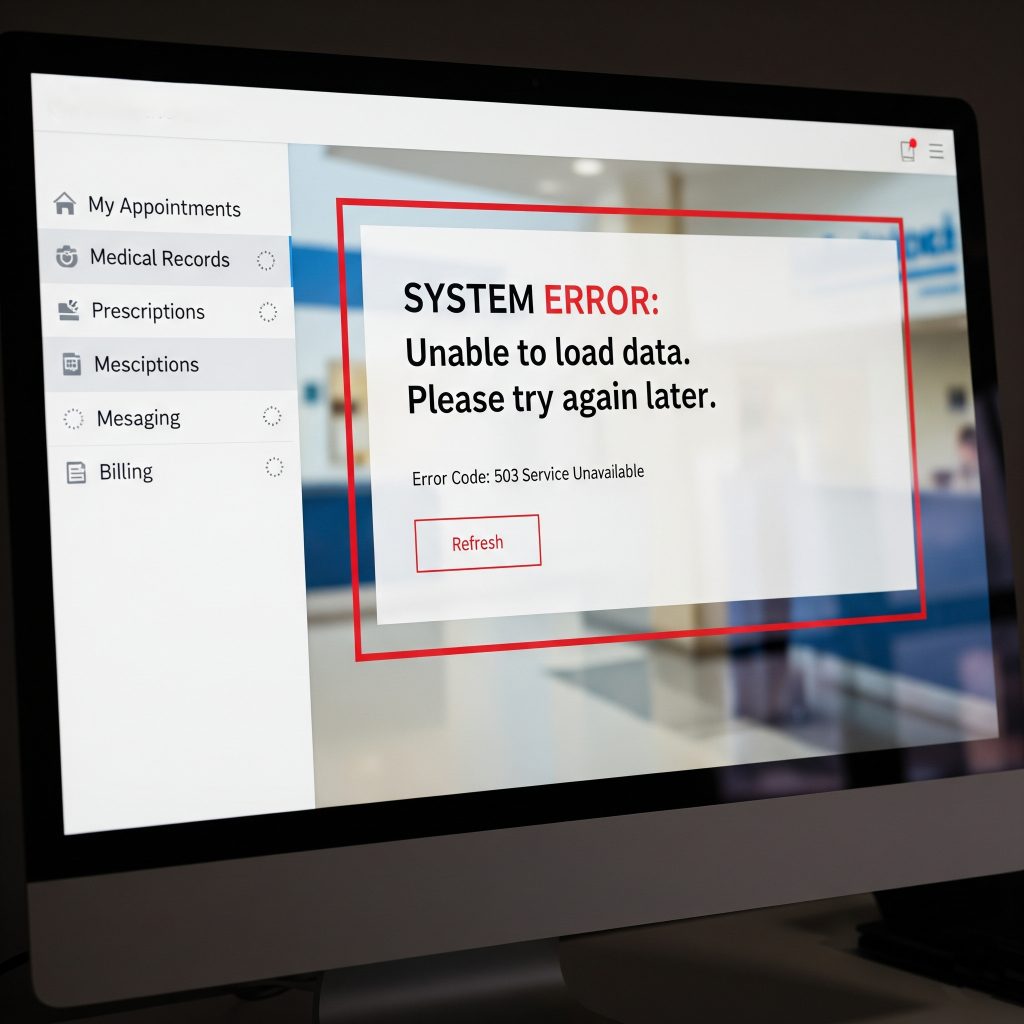
After 20 years in health plans, I’ve seen the same cycle repeat: We build better healthcare portals, yet members still don’t engage. We create intuitive dashboards, but satisfaction scores remain flat. We add features, and call volumes increase. The issue isn’t the interface—it’s the entire approach.
Menu-driven healthcare portals have a 23% (at best) completion rate for member tasks, while conversational interfaces achieve 67% completion rates. Yet, we keep investing millions in portal redesigns, wondering why members prefer calling our overwhelmed contact centers.
I’ve participated in countless “digital transformation” initiatives. I’ve attended hundreds of user experience sessions. I’ve watched focus groups struggle with “intuitive” interfaces. After two decades of incremental improvements, I can say this with certainty:
We’ve been solving the wrong problem.
The Portal Paradox: Better Design, Worse Outcomes
When I began in healthcare marketing in 2004, our member portal didn’t exist. A few years later, it was a simple digital brochure. Members could view their ID card and find basic plan information. It was clunky, but expectations were low.
Fast forward to 2025: Portals are design marvels—mobile-responsive, accessibility-compliant, user-tested interfaces that would impress Silicon Valley. Yet, member engagement rates have declined in many categories over the past five years.
How is this possible?
The answer lies in what I call the “cognitive load trap.” As healthcare became more complex—value-based care, narrow networks, prior authorizations, telehealth options—we responded by adding more features to our portals. More menus, more decision trees, more self-service options.
We assumed that giving members more control would increase satisfaction. Instead, we created digital mazes that require healthcare literacy, technical proficiency, and unlimited patience to navigate.
Consider this real scenario I witnessed recently: A 45-year-old member with diabetes needed to find an endocrinologist. Her journey through the portal looked like this:
- Log in (forgot password, reset required)
- Navigate to “Find a Provider”
- Select specialty from dropdown (40+ options)
- Enter location preferences
- Apply filters (accepting new patients, languages, hospital affiliations)
- Review 23 results
- Click individual profiles to check availability
- Cross-reference with her prescription coverage
- Verify the provider accepts her specific plan tier
- Attempt to schedule online (not available)
- Call the number provided (busy signal)
- Give up and call member services
Total time invested: 47 minutes. Outcome: Frustrated member, another call center interaction.
The Member Perspective Crisis
From the member’s perspective, healthcare portals aren’t helpful tools—they’re digital obstacles between them and the care they need. Our CAHPS data consistently shows this disconnect:
- 34% of members report difficulty finding information on health plan websites.
- 67% say they would prefer to “just ask someone” rather than navigate menus.
- Member satisfaction scores for digital interactions lag 23 points behind phone interactions.
But here’s what the data doesn’t capture: the emotional toll of digital healthcare friction.

I’ve read thousands of member comments over the years. The frustration isn’t just about usability—it’s about feeling abandoned in their moment of need. When a 68-year-old Medicare member is trying to understand their cancer treatment coverage at 2 AM, they don’t want to decode our perfectly designed information architecture. They want reassurance, guidance, and answers.
The portal paradigm assumes members want to become healthcare navigation experts. They don’t. They want to get healthy and get on with their lives.
This disconnect shows up in our operational metrics too. Despite billions invested in self-service portals, call center volumes haven’t decreased—they’ve shifted. Instead of calling to ask simple questions, members now call after exhausting themselves trying to find answers online.
“I spent an hour on your website and I still don’t know if my doctor is covered,” is the new standard opening line for member service calls.
The Cost of Clicks
The financial impact of our click-driven approach is staggering. Here are some numbers that should keep every health plan CFO awake at night:
Digital Transaction Costs:
- Average cost per successful portal transaction: $12-15 (including development, maintenance, and user support).
- Average cost per incomplete portal session that converts to a phone call: $35-40.
- Member acquisition cost lost to digital frustration: $250-400 per churned member.
Administrative Burden:
- 67% of portal “failures” result in phone calls within 24 hours.
- Average call handle time increases by 3.2 minutes when members have already attempted self-service.
- Customer service representatives spend 40% of their time walking members through portal functions.
Quality Impact:
- Members who struggle with digital interactions are 34% less likely to complete preventive care measures.
- HEDIS scores correlate negatively with portal complexity ratings.
- CAHPS communication scores drop 15-20% for plans with high digital friction.
The cruel irony? We built self-service portals to reduce costs and improve member experience. Instead, we’ve created expensive systems that generate more costly human interactions while frustrating the people we’re trying to serve.
But here’s the insight that changed everything for me: The problem isn’t that members don’t want to engage digitally. The problem is that we’ve been asking them to learn our language instead of speaking theirs.
The Breaking Point
Last year, during a member advisory board session, the plan showcased a newly redesigned portal, proud of the improved navigation and streamlined workflows. The feedback was swift and unanimous:
“It’s beautiful, but I still don’t know how to use it.”
“Can’t I just tell you what I need?”
“Why do I have to know what you call things to find what I’m looking for?”
That last comment struck me like lightning. They spent millions perfecting information architecture, yet we still required members to translate their human needs into our system categories.
A member doesn’t wake up thinking, “I need to access my explanation of benefits.” They think, “I got this bill and I don’t understand why I owe $200.” But portals require them to know that their question lives under “Claims and Payments” > “EOB Documents” > “Search by Service Date.”
This is the fundamental flaw in menu-driven healthcare: We’ve optimized for our internal organization instead of member mental models.
The solution isn’t another portal redesign. It’s a fundamental shift from menu-driven to conversation-driven healthcare. Instead of asking members to navigate our categories, what if we let them simply tell us what they need?
The Conversation Revolution Begins
Three months ago, I experienced the future of member engagement. Working with one of the top AI partners in the world, I realized how a 72-year-old Medicare member could easily have this interaction:
Member: “I need to find a heart doctor near my daughter’s house in Phoenix who speaks Spanish.”
AI: “I can help you find a cardiologist. Let me search for Spanish-speaking providers in Phoenix. What’s the zip code where your daughter lives?”
Member: “85016”
AI: “I found three highly-rated cardiologists within 10 miles of that area who speak Spanish fluently. Dr. Martinez at Banner Heart Center has the highest patient satisfaction scores and can see new patients next week. Would you like me to check what days work best for you?”
Member: “Yes, I can do Tuesday or Wednesday mornings.”
AI: “Perfect. Dr. Martinez has availability Tuesday at 10 AM. I can schedule that for you right now and send the appointment details to your phone. I’m also arranging transportation through your plan’s medical transportation benefit. Is that helpful?”
Total time: 90 seconds. Outcome: Scheduled appointment, transportation arranged, satisfied member.
This isn’t science fiction. This is happening right now, and it’s going to transform everything we think we know about member engagement.
In my next blog, I’ll show you exactly how conversational AI is rewriting the rules of healthcare interaction—and why the plans that embrace this shift will leave everyone else behind.
Because after 20 years of watching members struggle with digital innovations, I can finally say this: The technology exists to make healthcare as easy as having a conversation with someone who actually understands what you need.
The question is: Will healthcare plans be ready for the conversation revolution?
FAQ:
Q1. Why are traditional healthcare portals failing?
Traditional portals suffer from low engagement because they rely on complex menus and decision trees. Members face “digital mazes” that require technical skills, healthcare literacy, and patience—leading many to give up and call support instead.
Q2. What is the ‘cognitive load trap’?
As healthcare grew more complex, portals added more menus and features. This increased mental effort for members, making navigation overwhelming instead of empowering.
Q3. What’s the difference in completion rates between portals and conversational interfaces?
Healthcare portals average a 23% completion rate, while conversational interfaces achieve around 67% completion rates, proving they are far more effective.
Q4. How do portals impact member satisfaction and call center operations?
-
34% of members struggle to find information on portals.
-
67% would rather “just ask someone.”
-
Call volumes remain high, with calls lasting 3.2 minutes longer if members tried the portal first.
-
Service reps spend 40% of their time walking members through portal functions.
Q5. What is the financial impact of failed portal interactions?
-
Successful portal transactions cost $12–$15.
-
Failed sessions that lead to calls cost $35–$40.
-
Frustrated members cost health plans $250–$400 per churned member.
Q6. Why do members find portals frustrating?
Members think in human terms (“I don’t understand why I owe $200”), but portals force them to learn internal categories (“Claims > EOB Documents”). This mismatch leaves members feeling unsupported and abandoned.
Q7. What’s the alternative to menu-driven healthcare portals?
The future lies in conversation-driven healthcare, powered by AI. Instead of navigating menus, members simply state their needs, and AI guides them to solutions—reducing friction, improving satisfaction, and cutting costs.
Q8. Is conversational AI in healthcare just a theory?
No, it’s already happening. AI can now help members find providers, schedule appointments, arrange transportation, and answer coverage questions—all in under two minutes, compared to nearly an hour with portals.





